- Home
-
About us
-
Product
-
Project
- Scientific exchange
- News
- Videos
-
Member Centre
- Contact
With the development of society and the progress of science and technology, the material living standard of human beings has been continuously improved. Obesity has become a global epidemic and seriously affects human health in the past decades.In 2017, ncD-RISC published a survey of global obesity data in the Lancet, showing that the number of obese adults worldwide has soared from about 100 million to 650 million in 40 years;
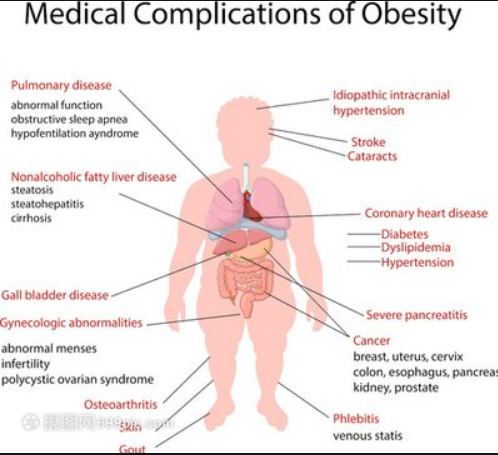 Figure 1 Represents the association between obesity and the onset of core disease over 40 years
Figure 1 Represents the association between obesity and the onset of core disease over 40 years
With the deepening and development of the understanding of obesity, people realize that obesity is not only weight gain, but also accompanied by a series of chronic syndromes, including type 2 diabetes, hypertension, sleep apnea, polycystic ovary syndrome.The association between obesity and cardiovascular disease is becoming increasingly clear;The risk of cardiovascular events increased significantly with an increase in body mass index (BMI), according to an epidemiological study that pooled data from 10 large prospective COHORT studies spanning 40 years of follow-up (1964-2015);
So we might ask some questions, why does obesity increase the risk of cardiovascular disease?What are the effects of weight loss therapy on cardiovascular disease?What are the effects of weight-loss medications on cardiovascular outcomes?With these three questions, we look at the results of various studies on the burden of obesity and related cardiovascular outcomes;
impact of obesity on the risk of cardiovascular disease: First, previous studies have shown that obesity is a recognized risk factor for atherosclerosis, ischemic heart disease, congestive heart failure and stroke,But we can't treat obesity as a single disease. Several studies have found that obesity can lead to more than 200 complications.Many of these complications, such as type 2 diabetes mellitus, non-alcoholic fatty liver disease and sleep apnea, are also risk factors for cardiovascular disease (CVD) 4,5.It is likely that obesity increases the risk of cardiovascular disease in part because of multiple complications;
So does obesity alone increase the risk of cardiovascular disease?Rishi Caleyachet of the University of Birmingham, UK, carried out a cohort study.He categorized the 3.5 million people without cardiovascular disease collected in the database between 1995 and 2015 by BMI and three metabolic abnormalities (diabetes, hypertension and hyperlipidemia),Cardiovascular events were observed and recorded during a mean follow-up of 5.4 years.Overweight and obesity were found to increase the risk of cardiovascular disease even in the absence of these three metabolic abnormalities (Figure 2);
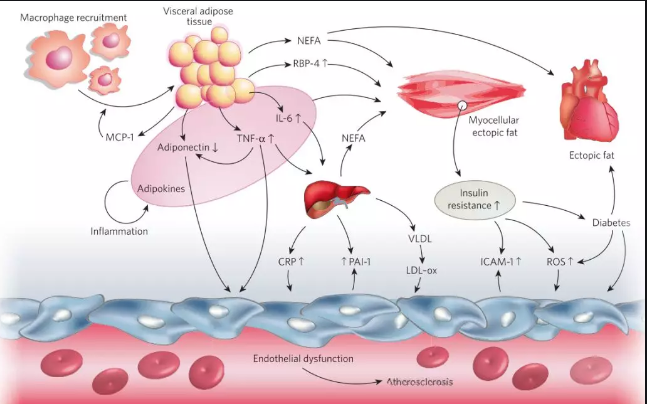
Figure 2 shows no metabolic abnormalities
Being overweight and obese also increases the risk of cardiovascular disease.So, what are the pathophysiological mechanisms by which obesity leads to an increased risk of cardiovascular disease?One of the core manifestations of obesity is the accumulation of fat,In addition to the increase of blood lipids, abnormal fat deposition can also cause pathophysiological changes including increased blood pressure, blood glucose, insulin resistance and abnormal inflammatory factors.These changes promote the expression of adhesion molecules, foam cell formation, smooth muscle proliferation, and lipid and cholesterol deposition on the vascular surface in all directions, promoting plaque formation and further altering arterial hemodynamics.The loss of elasticity of blood vessels and irregular shedding of plaque can "trigger" cardiovascular events at any time,Abnormal fat accumulation further increases the risk of cardiovascular events by promoting type 2 diabetes, non-alcoholic fatty liver disease, and cirrhosis (Figure 3);
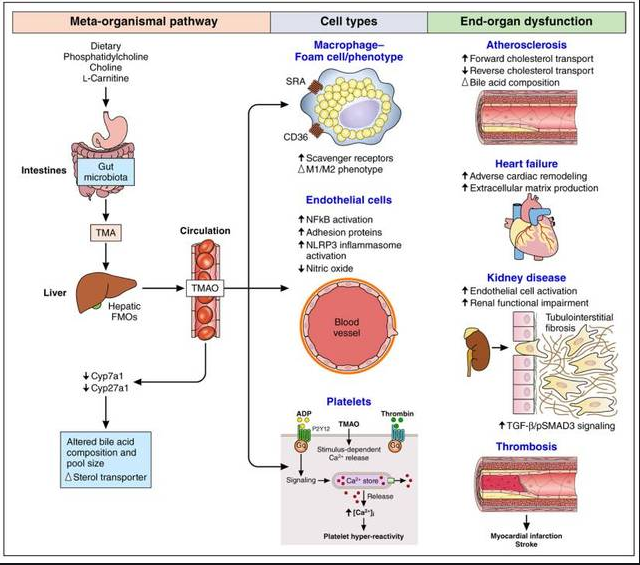 Figure 3 shows the key mechanisms of obesity-induced cardiovascular disease and related chronic diseases
Figure 3 shows the key mechanisms of obesity-induced cardiovascular disease and related chronic diseases
Effects of weight loss therapy on cardiovascular disease risk factors and outcomes: Based on the pathophysiological changes mentioned above, we will discuss the effects of weight loss on cardiovascular disease risk.A number of previous studies have shown that weight loss therapy can bring benefits such as lowering blood pressure, blood lipid and blood glucose, improving insulin resistance, and lowering the level of inflammatory factors, thus reducing the risk of cardiovascular disease;
Currently, the most common treatments for weight loss include lifestyle interventions, metabolic surgery and medication (Figure 4).In terms of weight loss, lifestyle interventions.Drug therapy;Metabolic surgery.Do they have the same effect on cardiovascular outcomes?
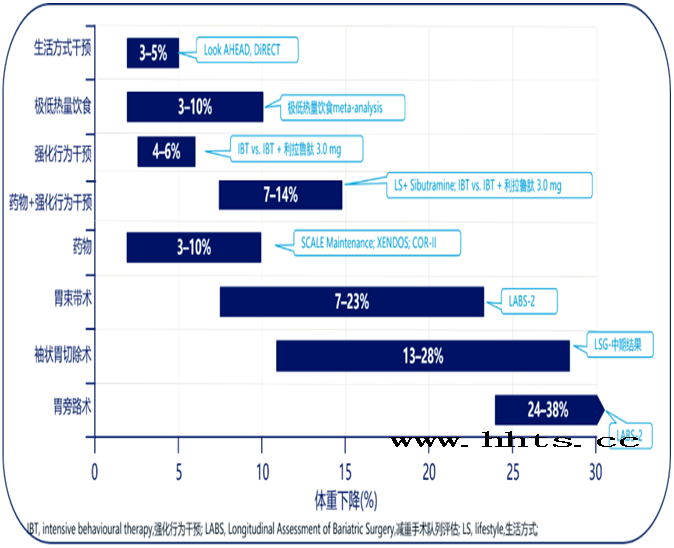
Figure 4 shows a summary of current studies on weight loss interventions and their efficacy results
Lifestyle interventions: The classic is the LookAHEAD study, funded by the National Institutes of Health.This is a prospective, multicenter, randomized, controlled clinical study to evaluate whether weight loss through intensive lifestyle interventions can reduce cardiovascular events and deaths in overweight or obese patients with type 2 diabetes;The final results suggest that intensive lifestyle interventions with the primary goal of weight loss do not reduce the incidence of cardiovascular events in overweight or obese adults with type 2 diabetes.Further post-mortem analysis revealed that a significant reduction in the risk of MACE was found only in patients who lost ≥10% of their body weight (Figure 5);
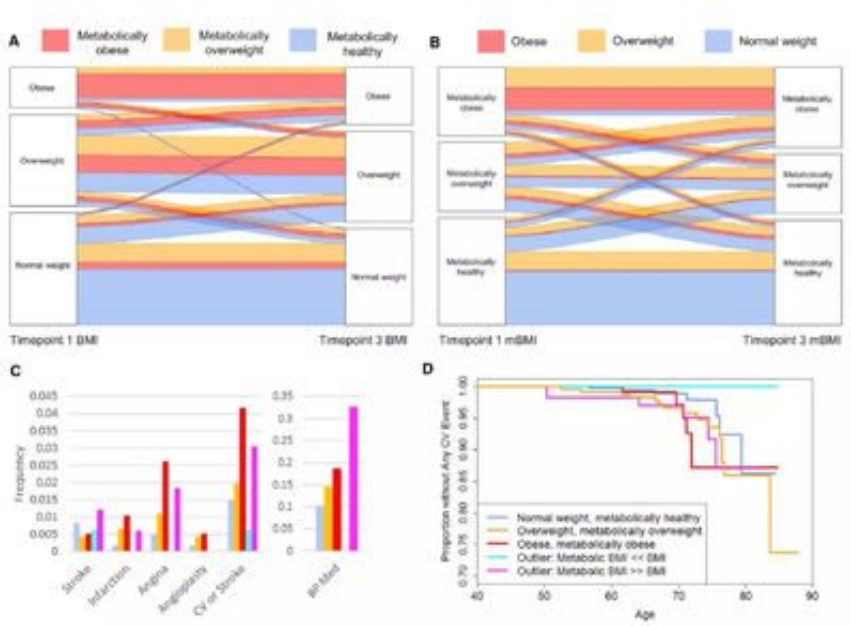 Figure 5 shows the Look AHEAD study and its post-analysis
Figure 5 shows the Look AHEAD study and its post-analysis
Among overweight/obese patients with type 2 diabetes, a significant reduction in the risk of MACE was found only in patients with ≥10% weight loss.The Daqing Study in China assessed the long-term effects of a 6-year lifestyle intervention trial (diet ± exercise) on impaired glucose tolerance in people with a mean BMI of 25.7 kg/m 2 (BMI& GT only;Encourage weight loss at 25 kg/m 2),During the 30-year follow-up of the Daqing study, the cumulative incidence of cardiovascular events was reduced by 26% in the lifestyle intervention group compared with the control group, including a 25% reduction in stroke, 27% reduction in coronary heart disease, and 29% reduction in heart failure;
Therefore, in obese/overweight patients with type 2 diabetes mellitus and abnormal glucose tolerance, lifestyle intervention can reduce the risk of cardiovascular disease to a certain extent;
Metabolic surgery: for patients with obesity that cannot be controlled by lifestyle interventions or medication (especially BMI>40 kg/m 2), metabolic surgery is the most effective treatment at present.Does metabolic surgery change the outcome of cardiovascular disease?
Swedish Obese Subjects (SOS) study compared two groups of obese patients who underwent routine treatment or bariatric surgery.After a median follow-up of 14.7 years, bariatric surgery significantly reduced the risk of cardiovascular death by 53%(P =0.002) and myocardial infarction or stroke by 33%(P<0.001);In another retrospective cohort study with a mean follow-up of 7.1 years, bariatric surgery reduced the risk of death in patients with coronary heart disease by 56% and in patients with type 2 diabetes by 92% compared with nonsurgical treatment in obese patients;
Weight loss drugs: Drug therapy has long been a popular treatment for obesity because it is more effective than lifestyle intervention in weight loss without the physical trauma associated with surgery.In contrast, in the history of more than 100 years, many weight-loss drugs have been withdrawn due to serious complications.Currently, weight-loss drugs can only be used as an adjunct to lifestyle therapy and are not recommended to be used alone;
Existing weight-loss drugs mainly work by regulating central appetite or/and peripheral digestion and absorption (Figure 6). Their efficacy has been shown in clinical trials, but what is their impact on the risk of cardiovascular disease?With the above questions in mind, we will introduce CVOT research as an important change in the development of weight-loss drugs;
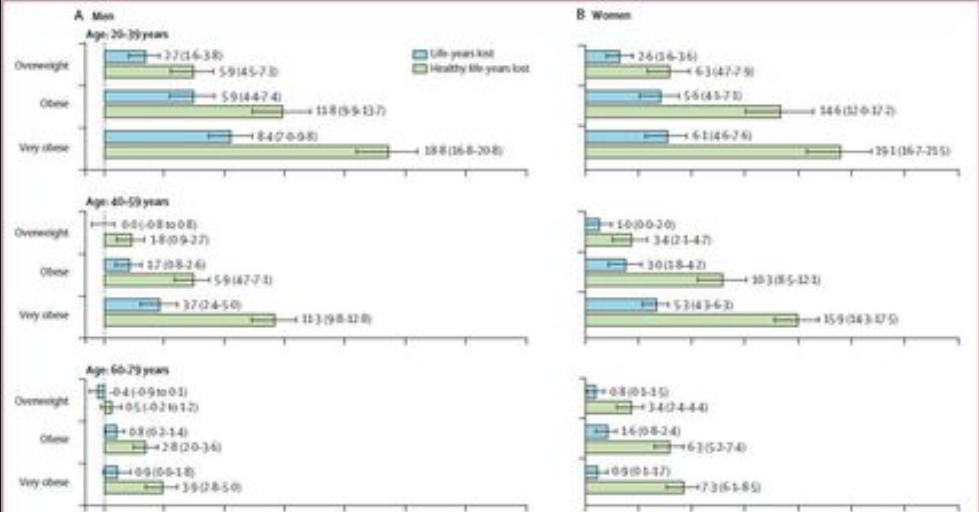 Figure 6 shows weight-loss drugs and their targets
Figure 6 shows weight-loss drugs and their targets
Study on the cardiovascular outcomes of weight-loss drugs: It is concluded that although weight-loss drugs can improve the risk factors of cardiovascular diseases such as body weight, blood lipid, blood pressure and blood sugar, not all weight-loss drugs can bring cardiovascular benefits;
The most typical is sibutramine, which has been associated with an increased risk of death from cardiovascular events since its introduction on the market.The SCOUT study, published in the New England Journal of Medicine in 2010, found that sibutramine significantly increased the risk of stroke and heart attack.That same year, the FDA held an advisory committee meeting and ultimately voted to remove sibutramine from the market;In 2012, the FDA issued "Cardiovascular Risk Assessment Requirements for Weight Loss Medications."In 2015, the European Medicines Agency (EMA) made similar recommendations.Since then, Cardiovascular Outcomes Trials (CVOT) have become a prerequisite for the marketing of weight-loss drugs;
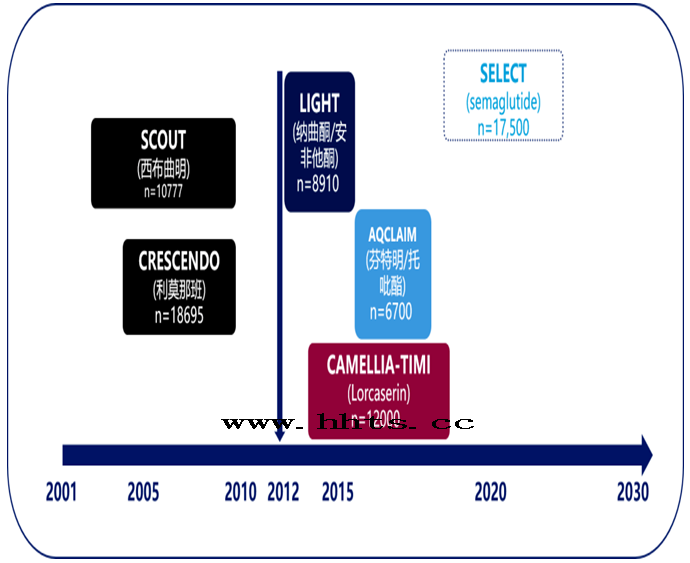 Figure 7 shows CVOT studies of weight-loss drugs since 2012
Figure 7 shows CVOT studies of weight-loss drugs since 2012
Camellia-timi61 is the only CVOT study completed since 2012.However, the results were non-inferiority, and based on the analysis of CVOT results of clocasserin, it was found that the clocasserin group had a higher incidence of tumor (7.7% vs 7.1%) and a tendency to cluster.Weighing the risks over the potential benefits, the FDA ordered it removed from the U.S. market in January 2020;
Based on these results, can we conclude that weight-loss drugs have no effect on cardiovascular risk?In recent years, glP-1RA has brought us a glimmer of hope with its remarkable efficacy in lowering glucose and weight in the field of diabetes,In the LEADER trial, 1.8 mg liraglutide reduced the risk of cardiovascular events in patients with type 2 diabetes, which was cited by regulators as evidence supporting the cardiovascular safety of 3.0mg liraglutide (note: Liraglutide 3.0mg has not yet been marketed in China, please refer to the Chinese manual for clinical use) 20;
A meta-analysis of data from seven glp-1ra CVOT studies conducted in patients with type 2 diabetes showed that glp-1ra significantly reduced the risk of MACE in patients at high risk of type 2 diabetes with CVD or CV, with baseline mean BMI>30 kg/m 2,Based on this, GLP-1RA has been studied in several clinical trials in obese/overweight people in recent years.If glP-1RA is proven to reduce the risk of MACE and provide cardiovascular benefits in future CVOT studies in obese/overweight patients, it is likely to be recommended by the guidelines;
Conclusion: Obesity and its complications are closely related to cardiovascular disease.
Weight loss therapy improves cardiovascular disease risk factors. Post-hoc analysis of lifestyle interventions in the Look AHEAD study and the SOS study of weight loss surgery showed partial cardiovascular benefits from weight loss;
Although clinical studies of bariatric agents have shown improvement in cardiovascular risk factors, no bariatric agents have been shown to be superior to placebo in the CVOT study to date;